Introduction
Both World Health Organization (WHO 5th) and International Consensus Classification (ICC) guidelines recognize mutations in nucleophosmin 1 ( NPM1mut) as a class defining molecular event in acute myeloid leukemia (AML). WHO 5th omitted the blast percentage requirement and ICC lowered the blast threshold to 10%. NPM1mut AML without FLT3 ITD or adverse risk cytogenetics is considered favorable risk in European LeukemiaNet (ELN) 2022, however co-occurring adverse-risk myelodysplasia related mutations (MR mut) do not influence ELN 2022 risk stratification. This analysis addresses the prognostic impact of blast enumeration in NPM1mut myeloid neoplasms (MN) with <10% blasts and influence of co-occurring mutations in NPM1mut AML.
Methods
We interrogated publicly available data from adult (≥18 years) patients (pts) with chronic myeloid neoplasms included in the International Working Group for Prognosis in MDS (N= 3,323; Bernard et al. NEJM Evid 2022) and two independent AML cohorts (AMLSG [N=1540] Papaemmanuil et al. NEJM 2016; UKNCRI [N=2,113] Tazi et al. Nat. Commun. 2022). Between group differences were assessed using the Wilcoxon rank-sum test or Fisher's exact test as appropriate. Time to event endpoints were analyzed using the log-rank method. Multivariate analysis (MVA) used cox proportional hazards regression.
Results
NPM1mut was identified in 17% (N=1148) of pts (AML: 30% [1109/3653], MN with <20% blasts: 1.2% [39/3,323]). Compared to pts with NPM1mut AML, pts with NPM1mut MN (MDS, CMML, aCML) with blast < 20% were older (median age 65 vs. 55 years, p < 0.001), had a lower median total WBC count (5 vs. 32 x10 9 /L, p < 0.001) and bone marrow (BM) blast percentage (8% vs. 76%, p < 0.001). No significant difference was observed between NPM1mut AML and MN with <20% blasts in median hemoglobin (9.1 vs. 9 x10 9, p: 0.44), platelets (62 vs. 66 x10 9 /L, p: 0.55), or NPM1mut variant allele frequency (VAF; 35% vs. 37%, p: 0.64).
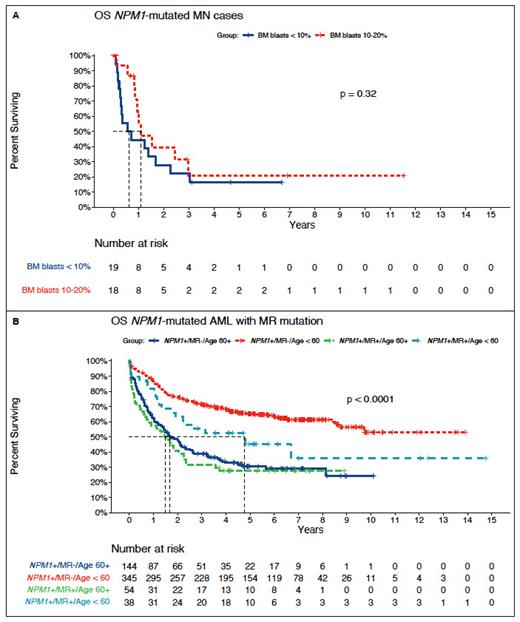
After a median follow up of 4.7 years (range: 0-12), no difference in overall survival (OS) was observed between pts with low blast (LB; <10%) NPM1mut MN (N=19) vs. ≥10% blasts (N=18) (median OS: 0.64 years [95% CI: 0.31-3.0] vs. 1.1 years [95% CI: 0.95-NR], p=0.32). Median leukemia free survival (LFS) was 0.81 years (95% CI: 0.67-1.5) and not significantly different between NPM1mut MN pts with <10 vs. ≥10% blasts (median LFS: 0.55 vs. 0.91 years, p=0.27).
In pts with NPM1mut AML (N=1109), 52% (N=581) were ELN 2022 favorable-risk; 15% (N=92) had MR mut including SRSF2 (51%, N=47), STAG2 (21%, N=19), ASXL1 (9%, N=8), BCOR (9%, N=8), RUNX1 ( 8%, N=7), EZH2 (5%, N=5), SF3B1 (5%, N=5), U2AF1 (1%, N=1), and ZRSR2 (1%, N=1). Pts with MR mut were older (median age 62 vs. 53 years, p < 0.001), had higher BM blasts (80% vs. 72% p=0.019), and lower platelets (45 vs. 77 x10 9/L p < 0.001) compared to pts with NPM1mut AML without MR mut. No significant difference in NPM1mut VAF was observed (34% in both groups).
After a median follow up of 3.5 years (range: 0-15), median OS was 6.2 years in pts with NPM1mut AML (95% CI: 4.2-9.7). Inferior OS was observed in ELN favorable risk NPM1mut pts with vs. without MR mut, respectively (2 vs. 8.4 years, p=0.0001). When stratified by age < 60 vs. ≥ 60 years, younger pts with MR mut had an increased risk of death (HR 1.7 95% CI: 1.1-2.8, p: 0.02). No OS difference was observed in older pts with or without MR mut (HR: 1.2, 95% CI: 0.80-1.68, p=0.44), however OS was significantly shorter in older pts with NPM1mut compared to younger pts (median 1.7 years vs. NR, p < 0.001). Patients with NPM1mut /MR mut AML had survival comparable to patients with ELN 2022 intermediate risk AML (2.0 vs. 2.1 years, p=0.35).
In MVA of NPM1mutAML adjusted for MR mut, BM blast percentage, age, performance status, baseline WBC, hemoglobin, platelet count, NPM1mut VAF, and treatment setting (AMLSG or UKNCRI), the presence of an MR mut (HR 1.39 [95% CI: 1.0-1.9], p=0.04), age < 60 (HR 0.43 [95% CI: 0.32-0.56], p < 0.001), and performance status (HR 1.35 [95% CI: 1.14-1.60], p=0.0004) retained statistical significance.
Conclusion
Pts with low blast NPM1mut MN have outcomes similar to pts with NPM1mut AML, supporting NPM1mut as an AML defining event irrespective of BM blast enumeration. In patients with ELN favorable risk NPM1mut AML, co-occurrence of MR mut is independently associated with inferior survival, comparable to ELN intermediate risk AML. These results may inform future refinements of current consensus guidelines.
Disclosures
Lachowiez:COTA Healthcare: Consultancy; Rigel Pharmaceuticals: Other: Advisory board. Bullinger:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene/BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees; Astellas: Honoraria; Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees; Jazz Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bayer Oncology: Research Funding; Pfizer: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria; Bristol-Myers Squibb: Honoraria; Daiichi Sankyo: Honoraria; Sanofi: Honoraria. Döhner:BMS: Consultancy, Research Funding, Speakers Bureau; Celgene: Consultancy, Research Funding, Speakers Bureau; CTI: Consultancy, Speakers Bureau; Novartis: Consultancy, Research Funding, Speakers Bureau; Roche: Consultancy, Speakers Bureau; Abbvie: Consultancy; Daiichi Sankyo: Consultancy; Janssen: Consultancy; Jazz: Consultancy; Astellas: Research Funding; Agios: Research Funding. Dohner:AbbVie: Consultancy, Research Funding; Agios: Consultancy, Research Funding; Amgen: Consultancy, Research Funding; Astellas: Consultancy, Research Funding; AstraZeneca: Consultancy; Berlin-Chemie: Consultancy; Bristol Myers Squibb: Consultancy, Research Funding; Celgene: Consultancy; GEMoaB: Consultancy; Gilead: Consultancy; Janssen: Consultancy; Jazz Pharmaceuticals: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Syndax: Consultancy; Kronos-Bio: Research Funding. Russell:Pfizer: Honoraria, Research Funding, Speakers Bureau; Jazz Pharma: Research Funding; Servier: Honoraria; Astellas: Honoraria. Loghavi:QualWorld: Consultancy; Guidepoint: Consultancy; Astellas: Research Funding; Amgen: Research Funding; Daiichi Sankyo: Consultancy; Caris Diagnostics: Consultancy; Gerson Lehrman Group: Consultancy; Abbvie: Consultancy; Blueprint Medicine: Consultancy; Recordati/ EUSA Pharma: Consultancy; Abbvie: Current equity holder in publicly-traded company. Papaemmanuil:TenSixteen Bio: Current equity holder in private company; Isabl Inc.: Current equity holder in private company, Current holder of stock options in a privately-held company, Other: CEO, Patents & Royalties: Whole genome cancer analysis.